https://www.propublica.org/article/...-inmates-to-avoid-paying-their-hospital-bills
Michael Tidwell’s blood sugar reading was at least 15 times his normal level when sheriff’s deputies took him to the hospital. But before they loaded the inmate into the back of a car, deputies propped up his slumping body and handed him a pen so he could sign a release from the Washington County Jail.
“I could barely stand up or keep my eyes open,” he recalled.
Tidwell said that he didn’t know what he was signing at the time, and that he lost consciousness a short time later. The consequences of his signature only became clear in the weeks that followed the 2013 medical emergency.
By signing the document, which freed him on bond from the small jail in south Alabama, Tidwell had in essence agreed that the Washington County Sheriff’s Office would not be responsible for his medical costs, which included the two days he spent in a diabetic coma in intensive care at Springhill Medical Center in Mobile.
It’s unclear whether Tidwell, who was uninsured at the time and in poor health afterward, was billed for his care or if the medical providers wrote it off. Neither Tidwell’s attorneys nor the hospital was able to say, and Tidwell was unable to get answers when he and a reporter called the hospital’s billing department.

Michael Tidwell at Springhill Medical Center in Mobile, Alabama. (Courtesy of Michelle Alford)
What is clear is that the sheriff’s office avoided paying Tidwell’s hospital bills.
Tidwell had been on the receiving end of a practice referred to by many in law enforcement as a “medical bond.” Sheriffs across Alabama are increasingly deploying the tactic to avoid having to pay when inmates face medical emergencies or require expensive procedures — even ones that are necessary only because an inmate received inadequate care while incarcerated.
What’s more, once they recover, some inmates are quickly rearrested and booked back into the jail from which they were released.
Local jails across the country have long been faulted for providing substandard medical care. In Alabama, for instance, a mentally ill man died from flesh-eating bacteria 15 days after being booked into the Mobile County Metro Jail in 2000. And in 2013, a 19-year-old man died of gangrene less than a month after he was booked into the Madison County Jail. In both cases, officials denied wrongdoing and surviving relatives settled lawsuits alleging that poor jail health care contributed to their loved ones’ deaths.
But the use of medical bonds isn’t about inferior care. It’s about who pays for care.
While medical bonds have been a last resort in many states for more than 20 years, experts say they are employed in Alabama more often than elsewhere. Their use in some counties but not in others illustrates the vast power and latitude that sheriffs have in Alabama, which is the subject of a yearlong examination by AL.com and ProPublica.
Several Alabama sheriffs, including Washington County Sheriff Richard Stringer, said in interviews that they often find ways to release inmates with sudden health problems to avoid responsibility for their medical costs. Stringer denied any wrongdoing in his office’s handling of Tidwell’s emergency.

Unchecked Power
The Extraordinary Power of Alabama Sheriffs
This article was produced in partnership with AL.com, which is a member of the ProPublica Local Reporting Network.
ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up for ProPublica’s Big Story newsletter to receive stories like this one in your inbox as soon as they are published.
Michael Tidwell’s blood sugar reading was at least 15 times his normal level when sheriff’s deputies took him to the hospital. But before they loaded the inmate into the back of a car, deputies propped up his slumping body and handed him a pen so he could sign a release from the Washington County Jail.
“I could barely stand up or keep my eyes open,” he recalled.
Tidwell said that he didn’t know what he was signing at the time, and that he lost consciousness a short time later. The consequences of his signature only became clear in the weeks that followed the 2013 medical emergency.
By signing the document, which freed him on bond from the small jail in south Alabama, Tidwell had in essence agreed that the Washington County Sheriff’s Office would not be responsible for his medical costs, which included the two days he spent in a diabetic coma in intensive care at Springhill Medical Center in Mobile.
It’s unclear whether Tidwell, who was uninsured at the time and in poor health afterward, was billed for his care or if the medical providers wrote it off. Neither Tidwell’s attorneys nor the hospital was able to say, and Tidwell was unable to get answers when he and a reporter called the hospital’s billing department.

Michael Tidwell at Springhill Medical Center in Mobile, Alabama. (Courtesy of Michelle Alford)
What is clear is that the sheriff’s office avoided paying Tidwell’s hospital bills.
Tidwell had been on the receiving end of a practice referred to by many in law enforcement as a “medical bond.” Sheriffs across Alabama are increasingly deploying the tactic to avoid having to pay when inmates face medical emergencies or require expensive procedures — even ones that are necessary only because an inmate received inadequate care while incarcerated.
What’s more, once they recover, some inmates are quickly rearrested and booked back into the jail from which they were released.
Local jails across the country have long been faulted for providing substandard medical care. In Alabama, for instance, a mentally ill man died from flesh-eating bacteria 15 days after being booked into the Mobile County Metro Jail in 2000. And in 2013, a 19-year-old man died of gangrene less than a month after he was booked into the Madison County Jail. In both cases, officials denied wrongdoing and surviving relatives settled lawsuits alleging that poor jail health care contributed to their loved ones’ deaths.
But the use of medical bonds isn’t about inferior care. It’s about who pays for care.
While medical bonds have been a last resort in many states for more than 20 years, experts say they are employed in Alabama more often than elsewhere. Their use in some counties but not in others illustrates the vast power and latitude that sheriffs have in Alabama, which is the subject of a yearlong examination by AL.com and ProPublica.
Several Alabama sheriffs, including Washington County Sheriff Richard Stringer, said in interviews that they often find ways to release inmates with sudden health problems to avoid responsibility for their medical costs. Stringer denied any wrongdoing in his office’s handling of Tidwell’s emergency.
Get Our Top Investigations
Subscribe to the Big Story newsletter.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
“We had a guy a couple of weeks ago with congestive heart failure. … The judge let him make bond so the county didn’t get stuck with that bill,” Lamar County Sheriff Hal Allred said in a March telephone interview. “We don’t have any medical staff in the jail. I wish we did, that would be great, but the way the county finances are, I won’t live long enough to see it.”
Typically the process works like this: When an inmate awaiting trial is in a medical crisis, a sheriff or jail staffer requests that a judge allow him or her to be released on bond just before, or shortly after, the inmate is taken to a hospital. If the request is granted, the inmate typically signs the document granting the release.
Michael Jackson, district attorney for Alabama’s 4th Judicial Circuit, said he is aware of multiple recent cases in which sheriffs released inmates on bond without first obtaining a judge’s approval. Jackson said he also worries about the risk of inmates reoffending after they receive medical treatment.
“I’m not saying there should be no situation where an inmate can get released early, but it shouldn’t be about money,” Jackson said in a phone interview this month. “No one’s watching them when they get out, and people might get robbed or their houses might get broken into.”
While judges usually sign off on bonds, lawyers who represent inmates and other experts say sheriffs are often the key decision-makers and can be held legally responsible for what happens after they release inmates via such methods.
If an inmate is already sick or injured when he or she is released, sheriffs are “not going to be able to avoid the liability just by opening the trap door and letting them go,” said Henry Brewster, one of Tidwell’s attorneys.
“They Have to Do Something”
Shortly after Tidwell was locked up for a probation violation in 2013, his sister Michelle Alford, a nurse at a Mobile hospital, said she brought his diabetes medications to the Washington County Jail and gave them to the guard on duty.
She says she explained to the staff that her brother is a “brittle” diabetic, meaning he needs frequent monitoring. She provided the jail with a two-page document that explained how often his blood sugar needed to be checked, what symptoms to watch for and the purpose of each medication.
The jail’s employees, none of whom had any formal medical training, did not follow those instructions, according to Tidwell’s jailhouse medical records, a copy of which Alford provided to AL.com and ProPublica.
On his fourth day in the aging jailhouse, Tidwell became ill and vomited off and on for the ensuing 48 hours. He was unconscious for most of his final two days there, according to court and medical records.

Tidwell ended up going to Springhill after his release on a medical bond. (Lynsey Weatherspoon for ProPublica)
Before he was taken to Washington County Hospital, Tidwell’s blood sugar reading was 1,500 mg/dl; a normal reading for him is 80 to 100 mg/dl. Over the less than seven full days he was incarcerated, he had lost at least 17 pounds, records show.
Tidwell’s release form bears his signature scrawled incomprehensibly outside the signature box, overlapping the typed prompt for “Signature of Defendant.” It does not match other examples of his signature on court documents reviewed by AL.com and ProPublica.
“If you’re in there and you get sick, they have to do something and get some medical attention,” he said. “But if you’re in so bad of shape that they’re trying to hold you up and get you to sign something, that’s wrong.”
Tidwell, who was 42 at the time, was assessed at the local hospital and taken to Springhill, a larger and better-equipped hospital, where he lay in a coma in the intensive care unit. He was suffering from renal failure and other complications related to his diabetes, according to the records.
During a conversation in his office in downtown Chatom, Stringer, the Washington County sheriff, said that he and his jail staffers are not medically trained. Instead, they “listen to what [inmates are] complaining about and examine them to determine if they need medical bond, because people will do anything to get out of jail.”
If they decide an inmate has a serious and potentially costly medical issue — and doesn’t pose a threat to the public — Stringer said he or the jail’s administrator will call a judge and request that the inmate be released.
Asked last week whether he believes Tidwell was legally able to provide consent to being bonded out, Stringer said: “They’ve got to be physically able to sign the bond. I’m sure he was [conscious] or he wouldn’t have been able to be bonded out. … It’s been so long ago it’s hard to remember all these things. I’m sure we did what needed to be done.”
But in an earlier interview, the sheriff provided an alternate explanation for Tidwell’s hospitalization.
“When someone comes in and says he’s a diabetic, we try to prepare a meal that will accommodate his diabetes,” Stringer said. “But now on commissary, they’re on their own there. I mean, you know you’re diabetic. Don’t order — he actually ordered 12 honey buns.”

Tidwell in an undated picture. (Courtesy of Michelle Alford)
Tidwell, who denies eating a dozen honey buns in the jail, recovered and was sent home from the hospital.
He filed a lawsuit against Stringer and several sheriff’s office employees in 2014; it was settled the following year. Stringer said he believes he and his employees would have been exonerated had the suit gone to trial, but because he said the settlement was for “something like $20,000 ... it’s not worth fighting it.”
But Tidwell’s problems didn’t end there. Exactly three months after Tidwell was released on bond, a judge issued a bench warrant for his arrest on another probation violation.
“They’ll Lower the Bond”
AL.com and ProPublica have reviewed the cases or media reports of inmates in 15 of Alabama’s 67 counties who were issued last-minute bonds or released on their own recognizance just before they were hospitalized for emergencies.
In September 2018, for instance, a 38-year-old inmate at the Lauderdale County Jail was taken to a nearby hospital after he suffered a stroke that left him partially paralyzed and unable to communicate verbally, stand or perform daily tasks, state court records show. The inmate, Scottie Davis, was released from sheriff’s office custody on bond the following day, though he couldn’t sign the release document. Someone instead wrote the words “Unable to sign due to medical cond.” in the space for the inmate’s signature. Davis was responsible for the medical costs after he was bonded out.
Lauderdale County Sheriff Rick Singleton said when inmates are too ill to sign their names, sheriff’s officials notify a judge who decides whether to allow them to be released on bond.
And earlier last year, in Randolph County, an inmate was released on a medical bond before going to the hospital for surgery, according to The Randolph Leader, a local newspaper. When he wasn’t able to immediately get the procedure, he was rearrested on a new misdemeanor charge and booked back into the Randolph County Jail.
The county ended up on the hook for the over $10,000 the procedure was expected to cost. Some county officials view the turn of events as an unfortunate financial setback.
Randolph County Commissioner Lathonia Wright said in a phone interview this month that paying inmates’ hospital bills is “really rough” on the county’s budget, but it sometimes can’t be avoided.
“I hate that we have to pay for it out of taxpayer money, but the law demands that we take care of people that are incarcerated in the jail,” he said. “If we get a bill, we pay for our medical bills. They come straight from the hospital.”
In urban counties with larger populations, the majority of inmates’ medical problems are dealt with in the jails, usually by private companies that provide infirmaries, round-the-clock nurses and doctors who make regular visits.
But in some rural counties, sheriffs do not have any staff members with medical training or the budget to absorb significant hospital costs.
Jim Underwood, who was sheriff of Walker County from 2015 until January, said the county budgeted about $350,000 per year for jail health care while he was in office. The sheriff’s office did everything it could to keep costs down, Underwood said, adding that before he was sheriff, one inmate’s medical care cost about $300,000.
“I think that a lot of it does depend on what they’re charged with … but there are people released because of medical bills,” he said. “You have to go through the judge; they’ll lower the bond.”
Underwood said he believes the practice “happens everywhere” in Alabama, though it takes different forms in different counties. One sheriff’s office has paid for inmates to wear ankle monitors while out on bond for unexpected medical care; another waited for an inmate’s relatives to secure a private bond before allowing him to be taken to a hospital, records show.
Sheriff’s officials in Washington County, where Tidwell was in custody, have faced other lawsuits alleging improper use of medical bonds, including in the case of a woman who died of a stroke one day after being released from the county’s jail in 2016. In that case, which was settled this year, an audio recording captured a top sheriff’s office official asking jail staff to ensure the woman was released on a medical furlough, a method of release similar to a medical bond, before taking her to the hospital.
Nora Demleitner, a law professor at Washington and Lee University in Virginia who specializes in criminal sentencing, said medical bonds may violate inmates’ rights and the way some sheriffs use them is “totally flawed.”
“It’s a stunning problem,” she said. “When [inmates] file lawsuits, and rightly so, they should get civil compensation.”
Demleitner added via email that the phenomenon is prevalent in a number of counties and entirely absent in others. AL.com and ProPublica have reviewed media reports of sheriffs pursuing medical bonds for inmates with medical crises in 25 states.
Alan Lasseter, a Birmingham-based attorney who has filed lawsuits over alleged police misconduct and jail health care issues, said sheriffs’ reliance on medical bonds appears to be on the rise.
“It’s only something I’ve been hearing about for about two years, maybe longer, but it’s becoming more common and it’s really starting to resonate with me that it’s been happening more and more in Alabama,” Lasseter said.
“They Are Responsible”
Marcus Echols said his daughter was 9 years old when he first learned that she was his child. Until then, the girl’s mother had been collecting child support from another man who was eventually determined not to be her father, according to court records and Echols.
In 1998, a judge in Morgan County ordered Echols to pay more than $9,000 worth of back child support and interest in monthly payments of $500.
Over the ensuing years, Echols, who pays support on other children and has had trouble keeping a job, repeatedly failed to make the required payments. By November 2015, when he was arrested for contempt of court for failure to make child support payments, his debt totaled more than $50,000. He was booked into the Morgan County Jail in Decatur, a city in north Alabama.
Two months later, on Jan. 16, 2016, Echols suffered a heart attack inside his painted cinder-block cell.
For over half an hour, guards argued over whether he needed to be taken to the hospital, Echols, now 49, said.
They eventually took him to Huntsville Hospital. Several hours later, Echols said, he awoke from a procedure and was told by a doctor that he had needed three stents inserted because his heart had suffered extensive damage over the extended period of time between when he went into cardiac arrest and his arrival at the hospital. Medical records reviewed by AL.com and ProPublica confirm Echols’ account of his condition and treatment.
The doctor also informed him that he had been officially released from Morgan County Sheriff’s Office custody, Echols said.
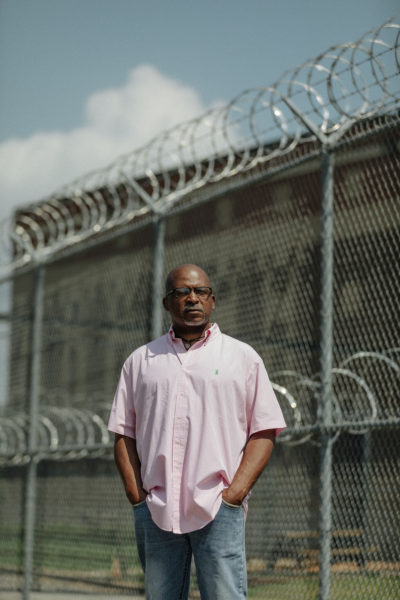
Marcus Echols outside the Morgan County Jail in Decatur, Alabama. (Lynsey Weatherspoon for ProPublica)
Echols said he was glad to find out that he would be allowed to go home instead of back to jail, but when he received a bill less than two weeks later from Huntsville Hospital for the costs of his medical care, he learned that he was personally responsible for more than $80,000.
“I didn’t get the bill until about a week after I got out of the hospital,” Echols said. “It just showed up in the mail.”
Echols said he never learned what mechanism the sheriff’s office had used to release him from its custody, and none of the court records associated with his lawsuit provide any clarity.
“I didn’t sign nothing. … When I woke up,” he said, “the doctor told me that the sheriff’s office had told him to tell me that I had been released from jail.”
A local charitable foundation ultimately paid Echols’ bills. But he still feels that he was taken advantage of.
“It seems like a scam that they’re running. They’re running the jail at the lowest possible cost at the expense of everyone else.”
Ana Franklin, who was sheriff at the time of Echols’ incarceration and hospitalization, declined to comment on Echols’ experience. But she said her “first consideration in whether or not to release someone on a medical release was never the budget.” She said the primary factors that drove such determinations when she was sheriff included criminal history, risk of reoffense and whether the jail was equipped to provide adequate medical care.
“It’s great to just say the sheriffs cut them loose because it saves them money on their medical,” said Franklin, who pleaded guilty last year to a federal charge of failing to file an income tax return. “But it’s just as big a liability issue that an inmate is going to say that we didn’t provide adequate treatment for them in the jail as it is that he’s going to sue us and say we cut him loose and they had to pay their medical bills.”
In March 2016, just a few weeks after Echols’ heart attack, the sheriff’s office attempted to obtain a new warrant to arrest him for contempt of court for his continued failure to pay the thousands of dollars worth of back child support he still owed.
Morgan County District Judge Charles B. Langham issued an order stating that Echols “is still under medical care” — he was attending cardiac rehab sessions at the time — and denied the sheriff’s office’s request. A year later, Langham issued an order for a new warrant for Echols’ arrest. At the time, Echols was unable to work, had applied for federal disability and was living with relatives.
Echols’ sister, Lashundra Craig, said she takes issue with the sheriff’s office’s persistent attempts to arrest her brother despite his continuing health issues.
“They are responsible for whatever happens to the inmates. … If they don’t want to be responsible for the medical costs but they want to put you back in jail to face your responsibility, to me it’s showing they just still want their money,” she said.
“They Said They Would Release Me”
It has historically been difficult for inmates to prevail in lawsuits alleging that sheriffs violated their rights by releasing them while they required medical attention.
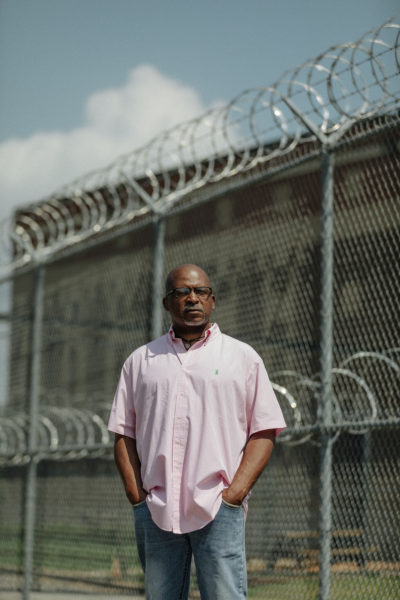
On July 3, 1996, four inmates beat Leroy Owens with a metal pipe; stabbed him with a screwdriver; kicked, stomped and punched him; and left him in a pool of blood in a common room on the second floor of the Butler County Jail in Alabama’s Black Belt.
Owens described the events of that evening in a recent interview, and they are laid out in detail in the records of the federal court case he and a fellow inmate who was also beaten would later file against then-sheriff Diane Harris, the county and the county commission in Alabama’s Middle District in Montgomery.
For nearly an hour, no one answered Owens’ cries for help or those of other inmates who banged on the jail’s walls, one of whom yelled, “They’re killing him up here,” according to the court records.
Finally, Harris’ chief deputy, Phillip Hartley, was called to the jail. Twenty minutes after the attack ended, Owens was taken downstairs and then driven to a nearby hospital, where he was treated for his injuries.
The hospital released Owens into the custody of two sheriff’s deputies, who were given a discharge document detailing “specific procedures to care for Owens’s head wounds and other injuries. It instructed them to monitor his level of consciousness, pupils, vision, and coordination, and to call the hospital immediately if any change occurred,” according to a summary of Owens’ allegations included in the U.S. Court of Appeals for the 11th Circuit’s ruling on the appeal of his federal case.
Instead, after they arrived at the jail, Hartley insisted that the bloodied inmate sign a bond granting his release, according to Owens and the court records.
“I signed out of the jail. All I know is it was a piece of paper I signed. I was bleeding and I was coming in and out of consciousness,” Owens, who is now 56, said last month. “They said they would release me if I signed it.”
After Owens signed the bond, Hartley drove him almost to the county line and dropped him off at about 3:30 a.m. on July 4, 1996, on the side of a desolate stretch of highway, without shoes, according to Owens and the court records.
“When he released me from the jail, he took me to the edge of the county and he said, ‘Your best bet is to leave town,’” Owens recalled.

Leroy Owens at a friend’s home in Mobile. The Butler County Sheriff’s Office took Owens to a hospital after he was attacked inside the county jail, but then bonded him out and left him shoeless on the side of the road. (Lynsey Weatherspoon for ProPublica)
After spending the night in a hotel, Owens awoke “in terrible pain” and was taken by ambulance back to the emergency room, according to the court records. He returned to the hospital again on July 8 for further treatment, the court records show.
Medicaid ultimately paid the hospital bills Owens incurred after he was bonded out from the jail.
Danny Bond, the current sheriff of Butler County, did not respond to repeated requests for comment.
In 2001, the 11th Circuit reinstated Owens’ case against the county, the sheriff and others after a lower court had dismissed it. The court ruled that though Owens and the other inmate did not prove that Harris or the county were deliberately indifferent to their medical needs, they “sufficiently stated a claim against the County and the Sheriff for the conditions at the Butler County Jail.” The court, however, also found that Harris was “entitled to immunity for her policy of releasing sick and injured inmates.”
Judge Rosemary Barkett, writing for a four-judge minority, disagreed, saying that the allegations of deliberate indifference against Harris should not be dismissed. Barkett wrote that Harris and her staff should have known that releasing Owens and leaving him on the side of the road after 3 a.m. could be a constitutional violation.
Harris and the county denied wrongdoing; Owens and the other inmate plaintiff ultimately settled the suit.
Meanwhile, legal experts who reviewed relevant portions of Alabama’s state code said they were able to find only two vague references to the issue: a statement that certain fees shall not be assessed “if a person is released on judicial public bail or on personal recognizance for a documented medical reason” and a stipulation that “the sheriff or jailer, at the expense of the county,” must provide “necessary medicines and medical attention to those who are sick and injured, when they are unable to provide them for themselves.”
Despite that, some lawyers and experts say inmates often have a hard time winning cases against sheriffs on those grounds.
“If a county sheriff threw someone out of the jail who’s unconscious and said ‘good luck,’ you could possibly make a civil rights violation or negligence claim,” said Paul Saputo, a Dallas-based criminal defense attorney who has represented multiple clients who have been bonded out of jail for medical reasons.
“If you have a heart attack and are taken to a hospital, and the question at the end of the day is who’s gonna pay for it, that’s a little bit closer of a call.”
“They’re Technically Still in Custody”
Lauderdale County, in Alabama’s northwest corner, has taken official action to expand the use of medical bonds.
During its April 25, 2017, meeting, the Lauderdale County Commission agreed to enter into a contract with a Tennessee company to provide ankle monitors and monitoring services for inmates who are permitted to leave the county’s jail to obtain expensive medical treatments.
Lauderdale County District Attorney Chris Connolly explained the concept during a discussion of the ankle monitor plan earlier that month, as Florence’s Times Daily newspaper reported at the time.
“Putting them on an ankle monitor and then releasing them on medical furlough or a recognizance bond would still allow us to have control of them, but also it would make them responsible for any medical treatment or expense,” Connolly said.
The new approach to reducing the jail’s medical costs has been used 12 to 15 times since the contract was signed, Singleton, the Lauderdale County sheriff, said in a telephone interview last month.
“I guess you’d consider it like house arrest,” he said. “They’re technically still in custody” and must immediately return to the jail once they are deemed healthy enough to do so. But instead of adding to the $500,000 of medical care the jail averaged annually as of 2017, the inmates must pay the bill. That means the program has been a success, according to Singleton.
“It’s accomplished what we wanted to accomplish,” he said. “It’s saved us some money.”
Singleton also emphasized that the program does not affect public safety because ankle monitors are only used in cases involving nonviolent inmates who are not considered threats to the community.
Lauderdale County District Judge Carole Medley, who rules on small-time criminal cases nearly every day in her courtroom, said she often grants bonds so inmates can obtain medical care, which they must then pay for themselves. She said that she is “very pro-ankle monitor,” and that she considers the program “a win-win” for inmates and for the jail and the county’s finances.
“I release people on [own recognizance] bonds every other week for medical issues. Do I take into consideration the charge? Of course. And there are times where we release them on an ankle monitor to get their medical needs addressed, and then some of them do return to jail.”
Critics of the practice say it raises important questions about the very purpose of incarceration. For instance, if sheriffs and other officials claim that these inmates must be jailed to prevent them from harming others, punish them for wrongdoing and deter would-be criminals, why are those officials so quick to abandon those goals in order to avoid paying their medical bills?
Jasmine Heiss, a campaign director at the Vera Institute of Justice in New York, said if such inmates can in fact be safely released when doing so saves tax dollars, perhaps they shouldn’t have been incarcerated in the first place.
“Broadly, what we would like to see is people who can be safely released on their own recognizance being released earlier in the process rather than waiting until people have these severe medical crises,” Heiss said.
Michael Tidwell’s blood sugar reading was at least 15 times his normal level when sheriff’s deputies took him to the hospital. But before they loaded the inmate into the back of a car, deputies propped up his slumping body and handed him a pen so he could sign a release from the Washington County Jail.
“I could barely stand up or keep my eyes open,” he recalled.
Tidwell said that he didn’t know what he was signing at the time, and that he lost consciousness a short time later. The consequences of his signature only became clear in the weeks that followed the 2013 medical emergency.
By signing the document, which freed him on bond from the small jail in south Alabama, Tidwell had in essence agreed that the Washington County Sheriff’s Office would not be responsible for his medical costs, which included the two days he spent in a diabetic coma in intensive care at Springhill Medical Center in Mobile.
It’s unclear whether Tidwell, who was uninsured at the time and in poor health afterward, was billed for his care or if the medical providers wrote it off. Neither Tidwell’s attorneys nor the hospital was able to say, and Tidwell was unable to get answers when he and a reporter called the hospital’s billing department.

Michael Tidwell at Springhill Medical Center in Mobile, Alabama. (Courtesy of Michelle Alford)
What is clear is that the sheriff’s office avoided paying Tidwell’s hospital bills.
Tidwell had been on the receiving end of a practice referred to by many in law enforcement as a “medical bond.” Sheriffs across Alabama are increasingly deploying the tactic to avoid having to pay when inmates face medical emergencies or require expensive procedures — even ones that are necessary only because an inmate received inadequate care while incarcerated.
What’s more, once they recover, some inmates are quickly rearrested and booked back into the jail from which they were released.
Local jails across the country have long been faulted for providing substandard medical care. In Alabama, for instance, a mentally ill man died from flesh-eating bacteria 15 days after being booked into the Mobile County Metro Jail in 2000. And in 2013, a 19-year-old man died of gangrene less than a month after he was booked into the Madison County Jail. In both cases, officials denied wrongdoing and surviving relatives settled lawsuits alleging that poor jail health care contributed to their loved ones’ deaths.
But the use of medical bonds isn’t about inferior care. It’s about who pays for care.
While medical bonds have been a last resort in many states for more than 20 years, experts say they are employed in Alabama more often than elsewhere. Their use in some counties but not in others illustrates the vast power and latitude that sheriffs have in Alabama, which is the subject of a yearlong examination by AL.com and ProPublica.
Several Alabama sheriffs, including Washington County Sheriff Richard Stringer, said in interviews that they often find ways to release inmates with sudden health problems to avoid responsibility for their medical costs. Stringer denied any wrongdoing in his office’s handling of Tidwell’s emergency.

Unchecked Power
The Extraordinary Power of Alabama Sheriffs
This article was produced in partnership with AL.com, which is a member of the ProPublica Local Reporting Network.
ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up for ProPublica’s Big Story newsletter to receive stories like this one in your inbox as soon as they are published.
Michael Tidwell’s blood sugar reading was at least 15 times his normal level when sheriff’s deputies took him to the hospital. But before they loaded the inmate into the back of a car, deputies propped up his slumping body and handed him a pen so he could sign a release from the Washington County Jail.
“I could barely stand up or keep my eyes open,” he recalled.
Tidwell said that he didn’t know what he was signing at the time, and that he lost consciousness a short time later. The consequences of his signature only became clear in the weeks that followed the 2013 medical emergency.
By signing the document, which freed him on bond from the small jail in south Alabama, Tidwell had in essence agreed that the Washington County Sheriff’s Office would not be responsible for his medical costs, which included the two days he spent in a diabetic coma in intensive care at Springhill Medical Center in Mobile.
It’s unclear whether Tidwell, who was uninsured at the time and in poor health afterward, was billed for his care or if the medical providers wrote it off. Neither Tidwell’s attorneys nor the hospital was able to say, and Tidwell was unable to get answers when he and a reporter called the hospital’s billing department.

Michael Tidwell at Springhill Medical Center in Mobile, Alabama. (Courtesy of Michelle Alford)
What is clear is that the sheriff’s office avoided paying Tidwell’s hospital bills.
Tidwell had been on the receiving end of a practice referred to by many in law enforcement as a “medical bond.” Sheriffs across Alabama are increasingly deploying the tactic to avoid having to pay when inmates face medical emergencies or require expensive procedures — even ones that are necessary only because an inmate received inadequate care while incarcerated.
What’s more, once they recover, some inmates are quickly rearrested and booked back into the jail from which they were released.
Local jails across the country have long been faulted for providing substandard medical care. In Alabama, for instance, a mentally ill man died from flesh-eating bacteria 15 days after being booked into the Mobile County Metro Jail in 2000. And in 2013, a 19-year-old man died of gangrene less than a month after he was booked into the Madison County Jail. In both cases, officials denied wrongdoing and surviving relatives settled lawsuits alleging that poor jail health care contributed to their loved ones’ deaths.
But the use of medical bonds isn’t about inferior care. It’s about who pays for care.
While medical bonds have been a last resort in many states for more than 20 years, experts say they are employed in Alabama more often than elsewhere. Their use in some counties but not in others illustrates the vast power and latitude that sheriffs have in Alabama, which is the subject of a yearlong examination by AL.com and ProPublica.
Several Alabama sheriffs, including Washington County Sheriff Richard Stringer, said in interviews that they often find ways to release inmates with sudden health problems to avoid responsibility for their medical costs. Stringer denied any wrongdoing in his office’s handling of Tidwell’s emergency.
Get Our Top Investigations
Subscribe to the Big Story newsletter.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
“We had a guy a couple of weeks ago with congestive heart failure. … The judge let him make bond so the county didn’t get stuck with that bill,” Lamar County Sheriff Hal Allred said in a March telephone interview. “We don’t have any medical staff in the jail. I wish we did, that would be great, but the way the county finances are, I won’t live long enough to see it.”
Typically the process works like this: When an inmate awaiting trial is in a medical crisis, a sheriff or jail staffer requests that a judge allow him or her to be released on bond just before, or shortly after, the inmate is taken to a hospital. If the request is granted, the inmate typically signs the document granting the release.
Michael Jackson, district attorney for Alabama’s 4th Judicial Circuit, said he is aware of multiple recent cases in which sheriffs released inmates on bond without first obtaining a judge’s approval. Jackson said he also worries about the risk of inmates reoffending after they receive medical treatment.
“I’m not saying there should be no situation where an inmate can get released early, but it shouldn’t be about money,” Jackson said in a phone interview this month. “No one’s watching them when they get out, and people might get robbed or their houses might get broken into.”
While judges usually sign off on bonds, lawyers who represent inmates and other experts say sheriffs are often the key decision-makers and can be held legally responsible for what happens after they release inmates via such methods.
If an inmate is already sick or injured when he or she is released, sheriffs are “not going to be able to avoid the liability just by opening the trap door and letting them go,” said Henry Brewster, one of Tidwell’s attorneys.
“They Have to Do Something”
Shortly after Tidwell was locked up for a probation violation in 2013, his sister Michelle Alford, a nurse at a Mobile hospital, said she brought his diabetes medications to the Washington County Jail and gave them to the guard on duty.
She says she explained to the staff that her brother is a “brittle” diabetic, meaning he needs frequent monitoring. She provided the jail with a two-page document that explained how often his blood sugar needed to be checked, what symptoms to watch for and the purpose of each medication.
The jail’s employees, none of whom had any formal medical training, did not follow those instructions, according to Tidwell’s jailhouse medical records, a copy of which Alford provided to AL.com and ProPublica.
On his fourth day in the aging jailhouse, Tidwell became ill and vomited off and on for the ensuing 48 hours. He was unconscious for most of his final two days there, according to court and medical records.

Tidwell ended up going to Springhill after his release on a medical bond. (Lynsey Weatherspoon for ProPublica)
Before he was taken to Washington County Hospital, Tidwell’s blood sugar reading was 1,500 mg/dl; a normal reading for him is 80 to 100 mg/dl. Over the less than seven full days he was incarcerated, he had lost at least 17 pounds, records show.
Tidwell’s release form bears his signature scrawled incomprehensibly outside the signature box, overlapping the typed prompt for “Signature of Defendant.” It does not match other examples of his signature on court documents reviewed by AL.com and ProPublica.
“If you’re in there and you get sick, they have to do something and get some medical attention,” he said. “But if you’re in so bad of shape that they’re trying to hold you up and get you to sign something, that’s wrong.”
Tidwell, who was 42 at the time, was assessed at the local hospital and taken to Springhill, a larger and better-equipped hospital, where he lay in a coma in the intensive care unit. He was suffering from renal failure and other complications related to his diabetes, according to the records.
During a conversation in his office in downtown Chatom, Stringer, the Washington County sheriff, said that he and his jail staffers are not medically trained. Instead, they “listen to what [inmates are] complaining about and examine them to determine if they need medical bond, because people will do anything to get out of jail.”
If they decide an inmate has a serious and potentially costly medical issue — and doesn’t pose a threat to the public — Stringer said he or the jail’s administrator will call a judge and request that the inmate be released.
Asked last week whether he believes Tidwell was legally able to provide consent to being bonded out, Stringer said: “They’ve got to be physically able to sign the bond. I’m sure he was [conscious] or he wouldn’t have been able to be bonded out. … It’s been so long ago it’s hard to remember all these things. I’m sure we did what needed to be done.”
But in an earlier interview, the sheriff provided an alternate explanation for Tidwell’s hospitalization.
“When someone comes in and says he’s a diabetic, we try to prepare a meal that will accommodate his diabetes,” Stringer said. “But now on commissary, they’re on their own there. I mean, you know you’re diabetic. Don’t order — he actually ordered 12 honey buns.”

Tidwell in an undated picture. (Courtesy of Michelle Alford)
Tidwell, who denies eating a dozen honey buns in the jail, recovered and was sent home from the hospital.
He filed a lawsuit against Stringer and several sheriff’s office employees in 2014; it was settled the following year. Stringer said he believes he and his employees would have been exonerated had the suit gone to trial, but because he said the settlement was for “something like $20,000 ... it’s not worth fighting it.”
But Tidwell’s problems didn’t end there. Exactly three months after Tidwell was released on bond, a judge issued a bench warrant for his arrest on another probation violation.
“They’ll Lower the Bond”
AL.com and ProPublica have reviewed the cases or media reports of inmates in 15 of Alabama’s 67 counties who were issued last-minute bonds or released on their own recognizance just before they were hospitalized for emergencies.
In September 2018, for instance, a 38-year-old inmate at the Lauderdale County Jail was taken to a nearby hospital after he suffered a stroke that left him partially paralyzed and unable to communicate verbally, stand or perform daily tasks, state court records show. The inmate, Scottie Davis, was released from sheriff’s office custody on bond the following day, though he couldn’t sign the release document. Someone instead wrote the words “Unable to sign due to medical cond.” in the space for the inmate’s signature. Davis was responsible for the medical costs after he was bonded out.
Lauderdale County Sheriff Rick Singleton said when inmates are too ill to sign their names, sheriff’s officials notify a judge who decides whether to allow them to be released on bond.
And earlier last year, in Randolph County, an inmate was released on a medical bond before going to the hospital for surgery, according to The Randolph Leader, a local newspaper. When he wasn’t able to immediately get the procedure, he was rearrested on a new misdemeanor charge and booked back into the Randolph County Jail.
The county ended up on the hook for the over $10,000 the procedure was expected to cost. Some county officials view the turn of events as an unfortunate financial setback.
Randolph County Commissioner Lathonia Wright said in a phone interview this month that paying inmates’ hospital bills is “really rough” on the county’s budget, but it sometimes can’t be avoided.
“I hate that we have to pay for it out of taxpayer money, but the law demands that we take care of people that are incarcerated in the jail,” he said. “If we get a bill, we pay for our medical bills. They come straight from the hospital.”
In urban counties with larger populations, the majority of inmates’ medical problems are dealt with in the jails, usually by private companies that provide infirmaries, round-the-clock nurses and doctors who make regular visits.
But in some rural counties, sheriffs do not have any staff members with medical training or the budget to absorb significant hospital costs.
Jim Underwood, who was sheriff of Walker County from 2015 until January, said the county budgeted about $350,000 per year for jail health care while he was in office. The sheriff’s office did everything it could to keep costs down, Underwood said, adding that before he was sheriff, one inmate’s medical care cost about $300,000.
“I think that a lot of it does depend on what they’re charged with … but there are people released because of medical bills,” he said. “You have to go through the judge; they’ll lower the bond.”
Underwood said he believes the practice “happens everywhere” in Alabama, though it takes different forms in different counties. One sheriff’s office has paid for inmates to wear ankle monitors while out on bond for unexpected medical care; another waited for an inmate’s relatives to secure a private bond before allowing him to be taken to a hospital, records show.
Sheriff’s officials in Washington County, where Tidwell was in custody, have faced other lawsuits alleging improper use of medical bonds, including in the case of a woman who died of a stroke one day after being released from the county’s jail in 2016. In that case, which was settled this year, an audio recording captured a top sheriff’s office official asking jail staff to ensure the woman was released on a medical furlough, a method of release similar to a medical bond, before taking her to the hospital.
Nora Demleitner, a law professor at Washington and Lee University in Virginia who specializes in criminal sentencing, said medical bonds may violate inmates’ rights and the way some sheriffs use them is “totally flawed.”
“It’s a stunning problem,” she said. “When [inmates] file lawsuits, and rightly so, they should get civil compensation.”
Demleitner added via email that the phenomenon is prevalent in a number of counties and entirely absent in others. AL.com and ProPublica have reviewed media reports of sheriffs pursuing medical bonds for inmates with medical crises in 25 states.
Alan Lasseter, a Birmingham-based attorney who has filed lawsuits over alleged police misconduct and jail health care issues, said sheriffs’ reliance on medical bonds appears to be on the rise.
“It’s only something I’ve been hearing about for about two years, maybe longer, but it’s becoming more common and it’s really starting to resonate with me that it’s been happening more and more in Alabama,” Lasseter said.
“They Are Responsible”
Marcus Echols said his daughter was 9 years old when he first learned that she was his child. Until then, the girl’s mother had been collecting child support from another man who was eventually determined not to be her father, according to court records and Echols.
In 1998, a judge in Morgan County ordered Echols to pay more than $9,000 worth of back child support and interest in monthly payments of $500.
Over the ensuing years, Echols, who pays support on other children and has had trouble keeping a job, repeatedly failed to make the required payments. By November 2015, when he was arrested for contempt of court for failure to make child support payments, his debt totaled more than $50,000. He was booked into the Morgan County Jail in Decatur, a city in north Alabama.
Two months later, on Jan. 16, 2016, Echols suffered a heart attack inside his painted cinder-block cell.
For over half an hour, guards argued over whether he needed to be taken to the hospital, Echols, now 49, said.
They eventually took him to Huntsville Hospital. Several hours later, Echols said, he awoke from a procedure and was told by a doctor that he had needed three stents inserted because his heart had suffered extensive damage over the extended period of time between when he went into cardiac arrest and his arrival at the hospital. Medical records reviewed by AL.com and ProPublica confirm Echols’ account of his condition and treatment.
The doctor also informed him that he had been officially released from Morgan County Sheriff’s Office custody, Echols said.
Marcus Echols outside the Morgan County Jail in Decatur, Alabama. (Lynsey Weatherspoon for ProPublica)
Echols said he was glad to find out that he would be allowed to go home instead of back to jail, but when he received a bill less than two weeks later from Huntsville Hospital for the costs of his medical care, he learned that he was personally responsible for more than $80,000.
“I didn’t get the bill until about a week after I got out of the hospital,” Echols said. “It just showed up in the mail.”
Echols said he never learned what mechanism the sheriff’s office had used to release him from its custody, and none of the court records associated with his lawsuit provide any clarity.
“I didn’t sign nothing. … When I woke up,” he said, “the doctor told me that the sheriff’s office had told him to tell me that I had been released from jail.”
A local charitable foundation ultimately paid Echols’ bills. But he still feels that he was taken advantage of.
“It seems like a scam that they’re running. They’re running the jail at the lowest possible cost at the expense of everyone else.”
Ana Franklin, who was sheriff at the time of Echols’ incarceration and hospitalization, declined to comment on Echols’ experience. But she said her “first consideration in whether or not to release someone on a medical release was never the budget.” She said the primary factors that drove such determinations when she was sheriff included criminal history, risk of reoffense and whether the jail was equipped to provide adequate medical care.
“It’s great to just say the sheriffs cut them loose because it saves them money on their medical,” said Franklin, who pleaded guilty last year to a federal charge of failing to file an income tax return. “But it’s just as big a liability issue that an inmate is going to say that we didn’t provide adequate treatment for them in the jail as it is that he’s going to sue us and say we cut him loose and they had to pay their medical bills.”
In March 2016, just a few weeks after Echols’ heart attack, the sheriff’s office attempted to obtain a new warrant to arrest him for contempt of court for his continued failure to pay the thousands of dollars worth of back child support he still owed.
Morgan County District Judge Charles B. Langham issued an order stating that Echols “is still under medical care” — he was attending cardiac rehab sessions at the time — and denied the sheriff’s office’s request. A year later, Langham issued an order for a new warrant for Echols’ arrest. At the time, Echols was unable to work, had applied for federal disability and was living with relatives.
Echols’ sister, Lashundra Craig, said she takes issue with the sheriff’s office’s persistent attempts to arrest her brother despite his continuing health issues.
“They are responsible for whatever happens to the inmates. … If they don’t want to be responsible for the medical costs but they want to put you back in jail to face your responsibility, to me it’s showing they just still want their money,” she said.
“They Said They Would Release Me”
It has historically been difficult for inmates to prevail in lawsuits alleging that sheriffs violated their rights by releasing them while they required medical attention.
On July 3, 1996, four inmates beat Leroy Owens with a metal pipe; stabbed him with a screwdriver; kicked, stomped and punched him; and left him in a pool of blood in a common room on the second floor of the Butler County Jail in Alabama’s Black Belt.
Owens described the events of that evening in a recent interview, and they are laid out in detail in the records of the federal court case he and a fellow inmate who was also beaten would later file against then-sheriff Diane Harris, the county and the county commission in Alabama’s Middle District in Montgomery.
For nearly an hour, no one answered Owens’ cries for help or those of other inmates who banged on the jail’s walls, one of whom yelled, “They’re killing him up here,” according to the court records.
Finally, Harris’ chief deputy, Phillip Hartley, was called to the jail. Twenty minutes after the attack ended, Owens was taken downstairs and then driven to a nearby hospital, where he was treated for his injuries.
The hospital released Owens into the custody of two sheriff’s deputies, who were given a discharge document detailing “specific procedures to care for Owens’s head wounds and other injuries. It instructed them to monitor his level of consciousness, pupils, vision, and coordination, and to call the hospital immediately if any change occurred,” according to a summary of Owens’ allegations included in the U.S. Court of Appeals for the 11th Circuit’s ruling on the appeal of his federal case.
Instead, after they arrived at the jail, Hartley insisted that the bloodied inmate sign a bond granting his release, according to Owens and the court records.
“I signed out of the jail. All I know is it was a piece of paper I signed. I was bleeding and I was coming in and out of consciousness,” Owens, who is now 56, said last month. “They said they would release me if I signed it.”
After Owens signed the bond, Hartley drove him almost to the county line and dropped him off at about 3:30 a.m. on July 4, 1996, on the side of a desolate stretch of highway, without shoes, according to Owens and the court records.
“When he released me from the jail, he took me to the edge of the county and he said, ‘Your best bet is to leave town,’” Owens recalled.

Leroy Owens at a friend’s home in Mobile. The Butler County Sheriff’s Office took Owens to a hospital after he was attacked inside the county jail, but then bonded him out and left him shoeless on the side of the road. (Lynsey Weatherspoon for ProPublica)
After spending the night in a hotel, Owens awoke “in terrible pain” and was taken by ambulance back to the emergency room, according to the court records. He returned to the hospital again on July 8 for further treatment, the court records show.
Medicaid ultimately paid the hospital bills Owens incurred after he was bonded out from the jail.
Danny Bond, the current sheriff of Butler County, did not respond to repeated requests for comment.
In 2001, the 11th Circuit reinstated Owens’ case against the county, the sheriff and others after a lower court had dismissed it. The court ruled that though Owens and the other inmate did not prove that Harris or the county were deliberately indifferent to their medical needs, they “sufficiently stated a claim against the County and the Sheriff for the conditions at the Butler County Jail.” The court, however, also found that Harris was “entitled to immunity for her policy of releasing sick and injured inmates.”
Judge Rosemary Barkett, writing for a four-judge minority, disagreed, saying that the allegations of deliberate indifference against Harris should not be dismissed. Barkett wrote that Harris and her staff should have known that releasing Owens and leaving him on the side of the road after 3 a.m. could be a constitutional violation.
Harris and the county denied wrongdoing; Owens and the other inmate plaintiff ultimately settled the suit.
Meanwhile, legal experts who reviewed relevant portions of Alabama’s state code said they were able to find only two vague references to the issue: a statement that certain fees shall not be assessed “if a person is released on judicial public bail or on personal recognizance for a documented medical reason” and a stipulation that “the sheriff or jailer, at the expense of the county,” must provide “necessary medicines and medical attention to those who are sick and injured, when they are unable to provide them for themselves.”
Despite that, some lawyers and experts say inmates often have a hard time winning cases against sheriffs on those grounds.
“If a county sheriff threw someone out of the jail who’s unconscious and said ‘good luck,’ you could possibly make a civil rights violation or negligence claim,” said Paul Saputo, a Dallas-based criminal defense attorney who has represented multiple clients who have been bonded out of jail for medical reasons.
“If you have a heart attack and are taken to a hospital, and the question at the end of the day is who’s gonna pay for it, that’s a little bit closer of a call.”
“They’re Technically Still in Custody”
Lauderdale County, in Alabama’s northwest corner, has taken official action to expand the use of medical bonds.
During its April 25, 2017, meeting, the Lauderdale County Commission agreed to enter into a contract with a Tennessee company to provide ankle monitors and monitoring services for inmates who are permitted to leave the county’s jail to obtain expensive medical treatments.
Lauderdale County District Attorney Chris Connolly explained the concept during a discussion of the ankle monitor plan earlier that month, as Florence’s Times Daily newspaper reported at the time.
“Putting them on an ankle monitor and then releasing them on medical furlough or a recognizance bond would still allow us to have control of them, but also it would make them responsible for any medical treatment or expense,” Connolly said.
The new approach to reducing the jail’s medical costs has been used 12 to 15 times since the contract was signed, Singleton, the Lauderdale County sheriff, said in a telephone interview last month.
“I guess you’d consider it like house arrest,” he said. “They’re technically still in custody” and must immediately return to the jail once they are deemed healthy enough to do so. But instead of adding to the $500,000 of medical care the jail averaged annually as of 2017, the inmates must pay the bill. That means the program has been a success, according to Singleton.
“It’s accomplished what we wanted to accomplish,” he said. “It’s saved us some money.”
Singleton also emphasized that the program does not affect public safety because ankle monitors are only used in cases involving nonviolent inmates who are not considered threats to the community.
Lauderdale County District Judge Carole Medley, who rules on small-time criminal cases nearly every day in her courtroom, said she often grants bonds so inmates can obtain medical care, which they must then pay for themselves. She said that she is “very pro-ankle monitor,” and that she considers the program “a win-win” for inmates and for the jail and the county’s finances.
“I release people on [own recognizance] bonds every other week for medical issues. Do I take into consideration the charge? Of course. And there are times where we release them on an ankle monitor to get their medical needs addressed, and then some of them do return to jail.”
Critics of the practice say it raises important questions about the very purpose of incarceration. For instance, if sheriffs and other officials claim that these inmates must be jailed to prevent them from harming others, punish them for wrongdoing and deter would-be criminals, why are those officials so quick to abandon those goals in order to avoid paying their medical bills?
Jasmine Heiss, a campaign director at the Vera Institute of Justice in New York, said if such inmates can in fact be safely released when doing so saves tax dollars, perhaps they shouldn’t have been incarcerated in the first place.
“Broadly, what we would like to see is people who can be safely released on their own recognizance being released earlier in the process rather than waiting until people have these severe medical crises,” Heiss said.