https://www.statnews.com/2017/09/21/sickle-cell-racism-doctors/
My medical school lesson was tinged with racism. Did that affect how I treated a sickle cell patient years later?
By JENNIFER ADAEZE OKWEREKWU @JenniferAdaeze
SEPTEMBER 21, 2017
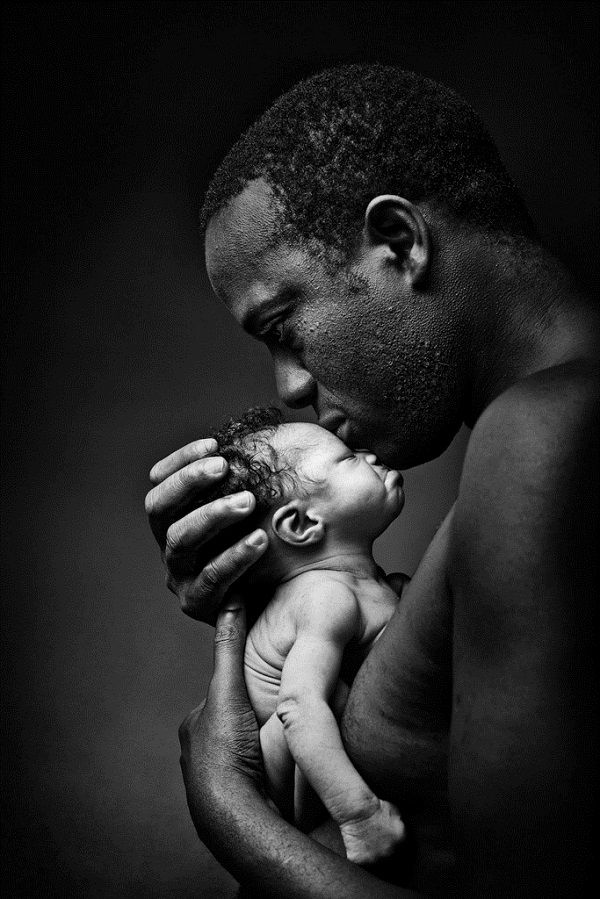
MIKE REDDY FOR STAT
T
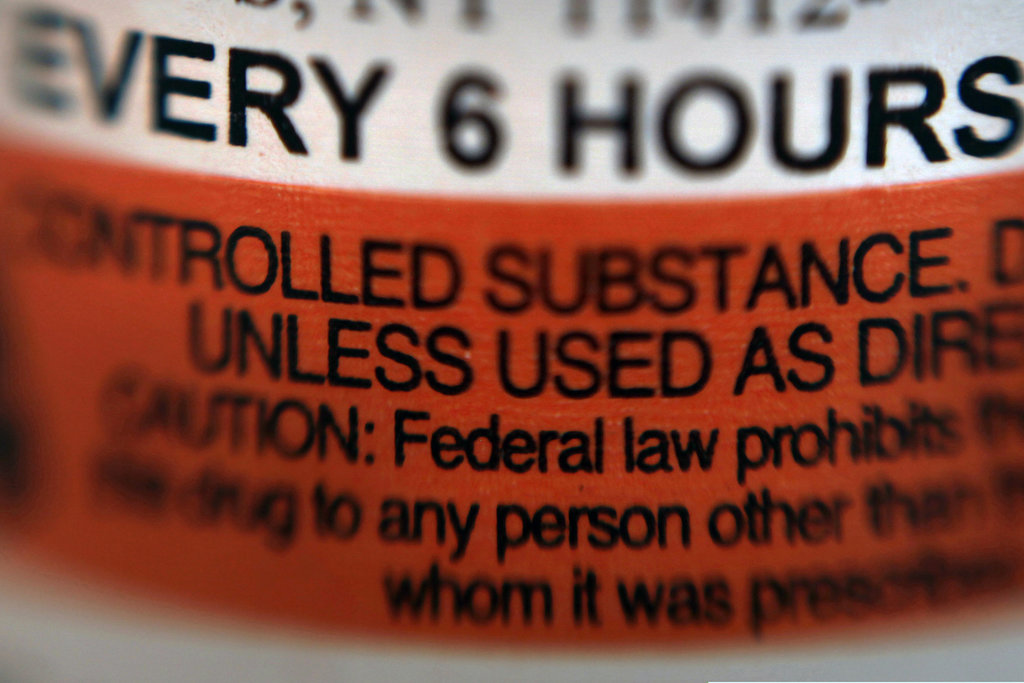
he young woman was curled up in a ball. She was sweating and shivering from pain. As she answered my questions — all my many, many questions — tears fell silently from her eyes.
I was a third-year medical student, and the resident I was working with had asked me to evaluate this woman. She had been here several times before. She was in the middle of a sickle cell crisis.
I remembered this young woman while reading
STAT’s recent story about how too many patients with sickle cell face exhausting, infuriating — and life-threatening — delays in getting care when they arrive in emergency rooms in excruciating pain from a restricted flow of oxygen to their organs.
ADVERTISEMENT
Thinking back, I’ve recognized the truth of that article: We don’t always take sickle cell seriously. I realized, too, that I, a doctor of color, might be complicit in bias against these patients. The more I think about it, the more I realize how deep the roots of that injustice stretch.

READ MORE
‘Every time it’s a battle’: In excruciating pain, sickle cell patients are shunted aside
In my first year of medical school, we learned about sickle cell — the genetics that lead to misshapen blood cells, and the damage such cells could do to the body. Our instructor mentioned that testing for sickle cell needed to be handled carefully, because they might become de facto paternity tests.
Such a statement could apply to other diseases with the same genetic inheritance patterns, such as cystic fibrosis or Tay-Sachs disease.
But we never talked about how testing for those diseases, which affect mostly whites, might lead to paternity shake-ups. That prospect was only mentioned with sickle cell — in a remark that carried a subtle indictment of a particular black family structure. Later, as my classmates and I talked about sickle cell in a discussion group, someone cracked a “baby-daddy” joke. Eventually, this
daytime TV clip, a staple of the talk show circuit, found its way around the entire class.
It was funny. I laughed. I hadn’t started seeing patients yet, so hadn’t yet experienced how such behavior could, in the long run, lead us to undermine some of our most vulnerable patients. I hadn’t yet realized how the insidious association between sickle cell and ridiculous paternity questions could make us internalize racially denigrating attitudes — and lead us to fail to take our patients seriously.
I didn’t have racist intent when I chuckled at that video. My classmates probably did not, either. But the tone set during that lesson on sickle cell may have affected how we all thought about the disease, and about our patients, for years to come.
We need to be sure that medical students learn about every disease without judging the people living with it.
NEWSLETTERS
Sign up for our hospitals newsletter, On Call
The sickle cell patient I evaluated in the hospital two years later was in bad shape. On top of her tears of pain, on top of the sweat and the shivering as her body revolted against her through no fault of her own, she had a fever and a cough. She needed fluids, pain medication, and oxygen at a minimum, and I planned to ask my resident to order these treatments. Slowly, I came to realize that she needed more than that: She had symptoms of acute chest syndrome, a leading cause of death for patients with sickle cell disease.
I quickly found my resident, apologized for interrupting the ultrasound he was doing, and said, “I think my patient has ACS.” I told him that I’d looked it up and learned that ACS requires prompt management to prevent death. “I think you should come look at her,” I said.
I was right. A chest X-ray confirmed the diagnosis and the woman was admitted to the hospital for treatment.
As sick as she was, why was I, a medical student, the first one to evaluate her? The emergency room triage system is supposed to send those in the most acute need to more experienced physicians. This patient had a long medical history of sickle cell-related issues and clearly needed urgent treatment by a knowledgeable clinician.
Yet she had ended up with me.
I had then compounded her misery — and perhaps put her life at risk — when, in trying to be a good medical student, I spent a lot of time asking her questions, and then spent even more time researching the complications of ACS before bringing my concerns to my supervisors.
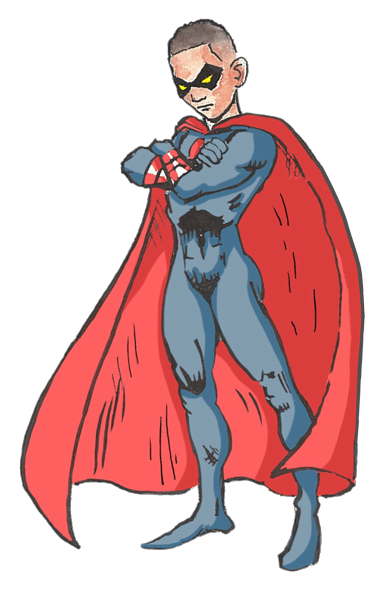
Why did I wait so long? Perhaps I trusted that my residents and attending physicians could accurately triage each patient’s risk, and would only allow me to practice my clinical skills alone in low-risk settings. Perhaps I wanted to prove that I could be compassionate but also clinically discerning — not get played by patients that were only after pain medications. Perhaps, I too had learned not to take this particular kind of suffering that seriously. I struggled with this existential crisis as I watched my patient with a sickle cell crisis get wheeled out of the emergency room on a hospital bed.

READ MORE
With a rapper’s death, harsh spotlight falls on slow progress against sickle cell
The message I took away: Her care was not a priority.
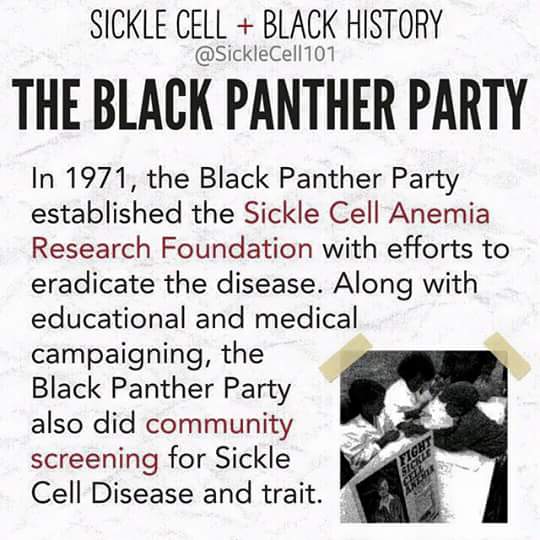
This attitude is pervasive from the bedside to the lab bench. Research on sickle cell disease
lags far behind. More people suffer from sickle cell than cystic fibrosis, but cystic fibrosis research gets 3.5 times the funding that sickle cell does.
Who decides what’s pressing and important? How do we communicate this urgency to the next generation of doctors and physician scientists in training?
If we are unable to challenge our attitudes and change our priorities, my fear is that we will continue to marginalize the care of these patients, especially in our efforts to curb the opioid epidemic. Deciding how to treat pain can be
really challenging, regardless of the diagnosis. But the question should never be one of deciding whose pain to treat and whose illness to take seriously.
As a doctor and a woman of color, I am renewing my commitment to treat all patients with equal dignity and concern. I hope I will continue to recognize when my attitudes have been wrongly shaped by racism, whether subtle or overt — and will continue to fight to avoid letting such views affect the way I practice medicine.