https://www.msn.com/en-us/news/us/f...laims-hampering-wildfire-response/ar-BB18WZ9G
New ads urge minorities to participate in coronavirus vaccine trials
http://a.msn.com/01/en-us/BB18WRZG?ocid=sf
https://twitter.com/share?url=http:...er=http://a.msn.com/01/en-us/BB18WRZG?ocid=st
https://web.whatsapp.com/send?text=http://a.msn.com/01/en-us/BB18WRZG?ocid=sw
As coronavirus vaccine trials struggle to get minority participation, a group formed by the National Institute of Allergy and Infectious Diseases has unveiled an ad campaign urging Black and Latino people to get involved.
The campaign, which includes television commercials and print ads, began to roll out earlier this week.
"This pandemic is not red. This pandemic is not blue. This pandemic is black, is brown, is white. It hits all colors and creeds," a voice-over on one ad says. "But even when things look bleak, we know that someone is full of hope and strength and wants to take action."
The ad features several people of different ethnicities. A second ad shared with NBC News includes a Black bus driver saying he's an essential worker and a Black restaurant worker saying he's a father. "That's why I volunteered," both men say.
The commercials, which were first reported by CNN, were developed by the Covid-19 Prevention Network, which, according to its website, was formed as a response to the pandemic and will help "conduct Phase 3 efficacy trials for COVID-19 vaccines and monoclonal antibodies."
Dr. Larry Corey, a virologist at Fred Hutchinson Cancer Research Center who leads the network, said it is crucial that the vaccine trials include minority volunteers.
“Our country and our global partners need vaccines against SARS-CoV-2 that are demonstrated to be safe and effective for everyone; so, it’s imperative that these vaccine trials are allowed to be conducted at the highest scientific standards and are inclusive of the people who have been most impacted by COVID-19,” he said in a statement Thursday to NBC News.
Corey said he believes the ad campaign "represents the most important voices in this fight" including essential workers, grandparents and food industry workers. "All of whom are feeling the impact of the pandemic every day and want to help find an answer to this ongoing restriction in our schools, travel and everyday life," he said.
Norbi Zylberberg, the founder of the advertising agency Socialisssima — which created the ads along with Sam Bonds Creative — said he hopes the ads give people a sense of hope.
The ads are “acknowledging what’s happening but giving people the choice to help, to roll up their sleeves," Zylberberg told NBC News in a phone interview Thursday. "But they're also explaining that the sooner we do that, the sooner we can go back to some normalcy.”
The television ads will run in both English and Spanish and will air on national networks as well as BET, the Oprah Winfrey Network, TV One, Telemundo and Univision.
Dr. Francis Collins, director of the National Institutes of Health, said at a Senate vaccine panel Wednesday that because the African American and Latino communities are the hardest hit by the coronavirus pandemic, it's important to know what benefits a vaccine will have on those groups.
"It’s without a doubt that there are also concerns in many of those communities about whether this is something they should trust to be in their best interest. There’s skepticism, there’s distrust," he said.
But "if we don’t succeed in having diversity in the participants in these trials, I think that takes scientifically away from the value of what we’re trying to learn," Collins added.
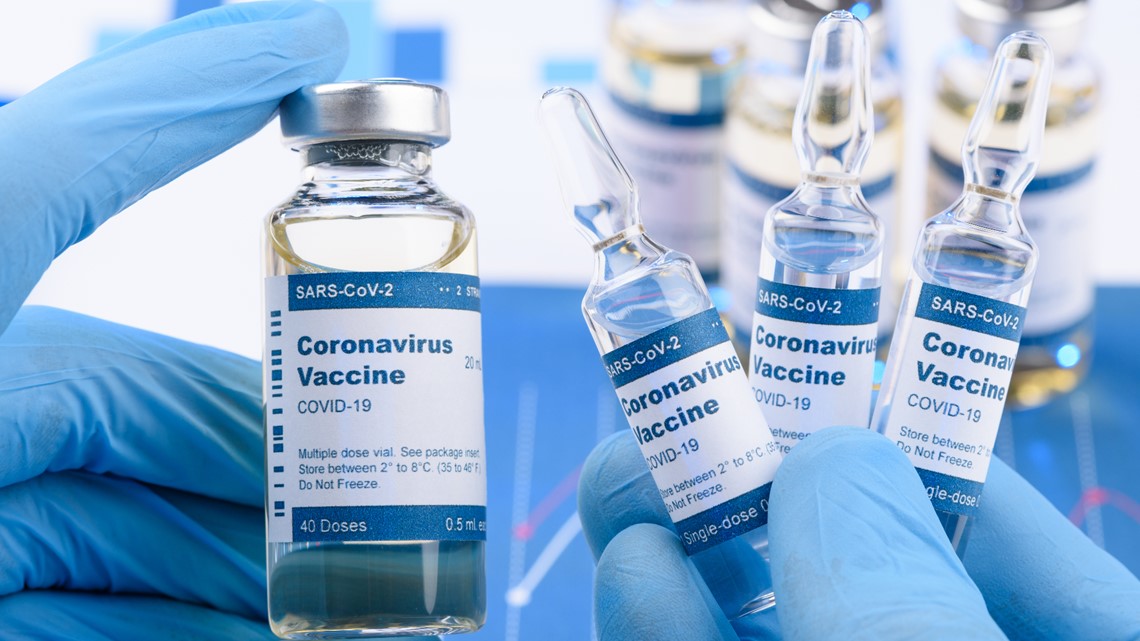
Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, told NBC News last week that without minority participation in the clinical trials, "you will not have definitively proven that the vaccine is safe and effective in them."
As of Sept. 4, roughly 26% of Moderna's participants were from "diverse communities," according to the website. Data shows that 10% of Moderna's new enrollments last week were Black and 16% were Hispanic or Latino, compared to 67% who were white. Pfizer's data shows that among its U.S. participants, 8% were Black and 11% were Latino.
The struggle to get minority involvement in the trials is layered. Some people are concerned that the White House is pushing the Food and Drug Administration to quickly approve a vaccine. Although Fauci had previously said that he believed a vaccine would likely be developed by the end of the year, DUMB ASS Donald Trump said during an August speech at the Republican National Convention that a vaccine was being produced "in record time" and promised to have a "safe and effective" vaccine this year.
Other concerns about the trials center around the infamous Tuskegee Syphilis Study, an experiment where Black men in Alabama were deliberately left untreated for syphilis and denied penicillin as treatment so government researchers could study the disease's effects. The study ran from 1932 to 1972.
While speaking with NBC News, Fauci said to try and calm minority groups who may be concerned about participating in the trials, "We need to make sure that we prove beyond a doubt that what we're doing is safe and effective."

 newsone.com
newsone.com
Scientists Conduct Consent-Free Experiments Disproportionately on Blacks, Study Says
The Tuskegee Experiment gave Black people a good reason to distrust what's happening.
Written By Nigel Roberts
Posted October 2, 2018
Given the African-American experience with the infamous Tuskegee experiment, it’s worrisome that the risks associated with consent-free experiments are not fairly spread out by race.
See Also: Blacks Underrepresented In ‘Life And Death’ Clinical Research, Study Finds
A study released on Monday found that African Americans are enrolled in clinical trials that don’t require patient consent at a disproportionately high rate, Stat News reported.
This involves administering experimental emergency medical procedures and drugs on patients who often can’t give consent because they’re unable to respond to questions. The Food and Drug Administration permits researchers to conduct these treatments under certain guidelines.
The study, published in Health Affairs, found that 29 percent of the patients involved in these experiments are Black, although African Americans represent about 13 percent of the population.
This stands in contrast to multiple studies that found African-Americans are underrepresented in consensual medical research. One study published in June, found that doctors have long used inaccurate guidelines to determine cardiovascular risks, which was particularly the case with at-risk African-Americans patients. A significant part of the problem with the guidelines was that Blacks were underrepresented in the patient sample used to create the guidelines.
News about consent-free experiments comes against the backdrop of government experiments, from 1932 to 1972, on African-American sharecroppers in Tuskegee, Alabama. Researchers deceived Black men about receiving treatment for syphilis, which actually went untreated. The experiments have contributed to widespread distrust in the African-American community of medical experiments—especially without consent.
The new study also revealed that many researchers who conduct consent-free experiments use a loophole to avoid publishing certain demographic data about the people they test. Government reporting regulations don’t specify which data they must reveal. This only adds to the lack of transparency and distrust.
New ads urge minorities to participate in coronavirus vaccine trials
http://a.msn.com/01/en-us/BB18WRZG?ocid=sf
https://twitter.com/share?url=http:...er=http://a.msn.com/01/en-us/BB18WRZG?ocid=st
https://web.whatsapp.com/send?text=http://a.msn.com/01/en-us/BB18WRZG?ocid=sw
As coronavirus vaccine trials struggle to get minority participation, a group formed by the National Institute of Allergy and Infectious Diseases has unveiled an ad campaign urging Black and Latino people to get involved.
The campaign, which includes television commercials and print ads, began to roll out earlier this week.
"This pandemic is not red. This pandemic is not blue. This pandemic is black, is brown, is white. It hits all colors and creeds," a voice-over on one ad says. "But even when things look bleak, we know that someone is full of hope and strength and wants to take action."
The ad features several people of different ethnicities. A second ad shared with NBC News includes a Black bus driver saying he's an essential worker and a Black restaurant worker saying he's a father. "That's why I volunteered," both men say.
The commercials, which were first reported by CNN, were developed by the Covid-19 Prevention Network, which, according to its website, was formed as a response to the pandemic and will help "conduct Phase 3 efficacy trials for COVID-19 vaccines and monoclonal antibodies."
Dr. Larry Corey, a virologist at Fred Hutchinson Cancer Research Center who leads the network, said it is crucial that the vaccine trials include minority volunteers.
“Our country and our global partners need vaccines against SARS-CoV-2 that are demonstrated to be safe and effective for everyone; so, it’s imperative that these vaccine trials are allowed to be conducted at the highest scientific standards and are inclusive of the people who have been most impacted by COVID-19,” he said in a statement Thursday to NBC News.
Corey said he believes the ad campaign "represents the most important voices in this fight" including essential workers, grandparents and food industry workers. "All of whom are feeling the impact of the pandemic every day and want to help find an answer to this ongoing restriction in our schools, travel and everyday life," he said.
Norbi Zylberberg, the founder of the advertising agency Socialisssima — which created the ads along with Sam Bonds Creative — said he hopes the ads give people a sense of hope.
The ads are “acknowledging what’s happening but giving people the choice to help, to roll up their sleeves," Zylberberg told NBC News in a phone interview Thursday. "But they're also explaining that the sooner we do that, the sooner we can go back to some normalcy.”
The television ads will run in both English and Spanish and will air on national networks as well as BET, the Oprah Winfrey Network, TV One, Telemundo and Univision.
Dr. Francis Collins, director of the National Institutes of Health, said at a Senate vaccine panel Wednesday that because the African American and Latino communities are the hardest hit by the coronavirus pandemic, it's important to know what benefits a vaccine will have on those groups.
"It’s without a doubt that there are also concerns in many of those communities about whether this is something they should trust to be in their best interest. There’s skepticism, there’s distrust," he said.
But "if we don’t succeed in having diversity in the participants in these trials, I think that takes scientifically away from the value of what we’re trying to learn," Collins added.
Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, told NBC News last week that without minority participation in the clinical trials, "you will not have definitively proven that the vaccine is safe and effective in them."
As of Sept. 4, roughly 26% of Moderna's participants were from "diverse communities," according to the website. Data shows that 10% of Moderna's new enrollments last week were Black and 16% were Hispanic or Latino, compared to 67% who were white. Pfizer's data shows that among its U.S. participants, 8% were Black and 11% were Latino.
The struggle to get minority involvement in the trials is layered. Some people are concerned that the White House is pushing the Food and Drug Administration to quickly approve a vaccine. Although Fauci had previously said that he believed a vaccine would likely be developed by the end of the year, DUMB ASS Donald Trump said during an August speech at the Republican National Convention that a vaccine was being produced "in record time" and promised to have a "safe and effective" vaccine this year.
Other concerns about the trials center around the infamous Tuskegee Syphilis Study, an experiment where Black men in Alabama were deliberately left untreated for syphilis and denied penicillin as treatment so government researchers could study the disease's effects. The study ran from 1932 to 1972.
While speaking with NBC News, Fauci said to try and calm minority groups who may be concerned about participating in the trials, "We need to make sure that we prove beyond a doubt that what we're doing is safe and effective."

Scientists Conduct Consent-Free Experiments Disproportionately on Blacks, Study Says
A study found that researchers disproportionately conduct consent-free experiments on Black people.
 newsone.com
newsone.com
Scientists Conduct Consent-Free Experiments Disproportionately on Blacks, Study Says
The Tuskegee Experiment gave Black people a good reason to distrust what's happening.
Written By Nigel Roberts
Posted October 2, 2018
Given the African-American experience with the infamous Tuskegee experiment, it’s worrisome that the risks associated with consent-free experiments are not fairly spread out by race.
See Also: Blacks Underrepresented In ‘Life And Death’ Clinical Research, Study Finds
A study released on Monday found that African Americans are enrolled in clinical trials that don’t require patient consent at a disproportionately high rate, Stat News reported.
This involves administering experimental emergency medical procedures and drugs on patients who often can’t give consent because they’re unable to respond to questions. The Food and Drug Administration permits researchers to conduct these treatments under certain guidelines.
The study, published in Health Affairs, found that 29 percent of the patients involved in these experiments are Black, although African Americans represent about 13 percent of the population.
This stands in contrast to multiple studies that found African-Americans are underrepresented in consensual medical research. One study published in June, found that doctors have long used inaccurate guidelines to determine cardiovascular risks, which was particularly the case with at-risk African-Americans patients. A significant part of the problem with the guidelines was that Blacks were underrepresented in the patient sample used to create the guidelines.
News about consent-free experiments comes against the backdrop of government experiments, from 1932 to 1972, on African-American sharecroppers in Tuskegee, Alabama. Researchers deceived Black men about receiving treatment for syphilis, which actually went untreated. The experiments have contributed to widespread distrust in the African-American community of medical experiments—especially without consent.
The new study also revealed that many researchers who conduct consent-free experiments use a loophole to avoid publishing certain demographic data about the people they test. Government reporting regulations don’t specify which data they must reveal. This only adds to the lack of transparency and distrust.