Children with Chronic Pain
How parents can help them to help themselves
Posted Oct 21, 2013
Taryn Oesch, who developed fibromyalgia at age 13, shared, “My mother forced me up and out, which was the last thing I wanted to do at that time! She’d get me to go for walks with her around the neighborhood, even though I complained the whole time.” Taryn, now in graduate school and working full time, credits her mother’s tenacity for her ability to return to high school (after a period of being home-bound) and to persevere. Her mother, who never doubted her daughter’s experience, heeded her doctor’s words that fibromyalgia would bring pain, whether Taryn was
lying on the couch or participating actively in life—and made it her mission to empower her daughter. This involved adaptation, such as having her daughter participate in physical therapy rather than gym class when she returned to school.
Taryn was lucky because her mother coached and encouraged her. However, even the best intentioned parents struggle with the
stress and uncertainty involved in caring for children who have
chronic pain.
Acknowledge the Difficulties
First of all, parents need to give themselves a break. Accepting that one’s child has a chronic
health problem of any kind is a difficult process. Witnessing your child suffering from pain, and associated losses, is understandably painful. A recent study shows that parents experience significant distress around the complex and counterintuitive decisions involved in caring for a child with chronic pain. [1]
Parents are often pulled with some immediacy into advocacy roles for their child, while at the same time, facing their own fears,
grief, losses, frustration,
anger, inadequacy, uncertainty, and powerlessness. Parents who initially misread their child’s behavior, such as not wanting to go to school, as a “phase,” willfulness, evidence of drug use, or other misinterpretation, may experience
shame. Parents who have a painful condition themselves may experience
guilt for passing along “responsible”
genes. Whatever the circumstances, diagnosis is seldom obvious or predictable, and illness is never anyone’s fault. It is important that parents acknowledge the challenge they face, make room for whatever feelings arise, and practice letting go of self-judgment. Parenting a child (including adult children) who suffers from chronic pain is difficult.
While the specifics may differ based on a child’s health condition, symptom severity, and treatment regimen, parents face questions about when to nurture and when to push. It makes sense that parents may want to shield their children from additional suffering, while worrying that too much insulation can interfere with their growth and development. Conflict over these competing desires can lead to inner turmoil, inconsistency, and also family discord when parents hold opposing views.
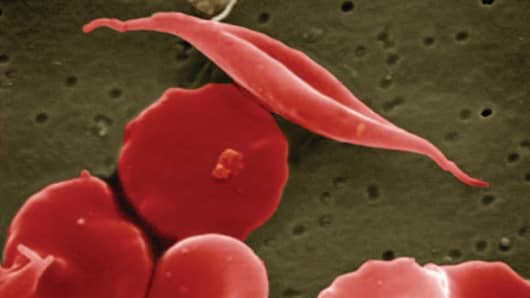
See your child, not the illness
Source:
Figuring out then to coddle and when to foster independence is a central task of
parenthood. This becomes additionally challenging when a child is ill. However, studies across a number of pain conditions have found that children fare best and are most adaptive when parents do not focus primarily on their child’s symptoms, allow too frequent avoidance of activities, or exhibit great distress themselves.[2,3,4] In other words, the less that parents emphasize their children’s difficulties the better. Consider how toddlers look expectantly to parents before committing to a reaction themselves. When toddlers stumble, for example, they quickly interpret parents’ verbal and nonverbal cues to assess whether to laugh it off and keep going, or howl until comforted.
Children with chronic illness benefit from parents’ normalizing the situation in an accepting, matter-of-fact way. This is different from ignoring or discounting reports of pain. Parents can acknowledge what a child expresses without escalating or reinforcing distress. Parents’ level of acceptance will come through.
Foster positive self-awareness
The inherent paradoxes of complex pain conditions require the ability to
act in counterintuitive ways, such as getting up and moving, despite pain and exhaustion, and also limiting activity, despite pain respites. Parents can help children make sense of their experience. Parent and child both can conduct experiments and develop a corresponding narrative.
article continues after advertisement
For example:
Notice times when your child can engage in activities that positively distract them from pain. Remark on them gently in the moment. Ask questions to understand your child’s experience. Then, use this information to help cultivate self-awareness about the variation of pain:
- “I know you hurt right now, and don’t feel up to seeing friends. However, last time you didn’t feel up to it, and then later told me that you had a great time with your buddies.”
You can add in more detail that you collect, such as:
- “It may not feel like it right now. But remember that you told me that your pain went down to a “2” (out of 10) when you were with friends? And it had started at an “8,” right?
Rather than giving the choice of whether or not to go, ask questions that foster problem solving:
- “What will help you enjoy yourself the most?”
It’s most effective when the child answers this for him or herself. Providing choices when possible can help children feel more responsible and in control.
Parents can plant seeds by sharing observations from comparable situations:
- “Didn’t you say that the seats in that movie theater were really comfortable?”
article continues after advertisement
Friendships are important. Help your child connect.
Source:
Encourage them to brainstorm about restorative activities they can enjoy when they return home, such as a hot bath, favorite music, or other pleasant experience. Knowing that something comforting awaits them can increase their willingness to take a risk and participate. This works both as an incentive and as positive behavioral shaping for self-care and balance.
Parents with pain conditions can model positive adaption through engagement and adaptation. How parents demonstrate coping, flexibility, and carving out restorative time to rejuvenate sends a powerful message.
Nurture self-expression
Source:
Research also shows that the less focused individuals are on symptoms, the better [2,3,4]. Consider ways to help children pursue their interests and passions and explore new ones. Attending to a child's pursuits and achievements reinforces the message that illness does not define them as a person. Practice gently encouraging them to participate, along with any positive adaptations, as needed. Keep it low key: “We can toss a soccer chair in the trunk just in case you need to take a break.”
article continues after advertisement
Validate the difficulties
While encouraging children to forge ahead, it is also essential that family members communicate their belief about the child's experience, including the severity of the pain. Taryn's story illustrates the importance of asking how the child feels and avoiding snap judgments. Given the invisibility of pain and the uniqueness of their situation (compared with peers), children will face disbelief from others.
Carve out moments to sit with your child and offer support. Practice putting words on their experience, without trying to problem-solve or encourage:
- “That sounds really hard.”
- “How frustrating.” “How sad.” and so on.
Naming emotions shows that you understand and helps them to develop ways to describe and understand their own experience.
Let your child know that you are able to handle hearing about difficulties. Children may or may not readily share, but will value the offer. Parents are in the position to provide unconditional support. Communicating openly and honestly in an age-appropriate way can also build trust and ease fears.
Self-care for parents
Imagining how your child may feel can build empathy; however, dwelling on it is destructive. Parents also need respite from thinking about pain. Research suggests that parental distress not only affects parents, but the child and entire family. [3]
Be deliberate in cultivating the positives in your own life. Engage in activities you find pleasurable, relaxing, and fulfilling. Look to and cultivate supportive relationships. Consider healthful choices that reduce your own vulnerability, such as by getting adequate
sleep,
nutrition, and exercise. Neglecting your own needs creates a negative feedback loop. In order to keep positive for your child, you, too, need to find ways to create reserves of positivity. Make time to do things you enjoy. Keep in mind that exercise and
laughtercan release tension and fortify you.
Watch out for the “shoulds,” such as:
- “I shouldn’t have fun if my child hurts.”
- “I shouldn’t complain about how I feel …”
Instead, look for ways to keep your child’s medical condition from overwhelming your own life, relationships, and family. Sometimes this requires being deliberate about carving out time for intimacy (“date night”), as well as “family time,” in which family members can connect over activities that everyone can enjoy. Spending time with each family member also reduces the risks associated with “well children,” whose needs can be overshadowed by an ill
sibling.
It is also vital to know your limits. Take “time outs” as needed. Do your best to figure out what is essential and to reward yourself along the way. Strive to be flexible, gentle, and
understanding with yourself too.
The value of support
Despite your best efforts, at times you will likely struggle with feeling ineffective, frustrated, disappointed, angry, or anxious. There is no need to do this alone.
Psychotherapy and support groups can offer support and coping skills to help you, your child, your relationship with a partner, or the family as a whole. One mother confided that her biggest regret was not seeking
counseling to help family members cope with difficulties. Professionals can help parents and children alike to sort out their feelings and find strategies to navigate their lives.
You can also look to parents and children who are going through the same thing for practical suggestions and support. Knowing that you are not alone is invaluable. At the same time, be careful to limit the extent to which you or your child may identify with an “illness community,” as this can narrow one’s
self-image. The goal is to figure out how to live as full and rich a life as possible. Connecting to the wider community (beyond illness) helps separate one’s identity from “illness” (which is just a facet of one’s experience). This is as important for a child as it is for parents and the entire family.
https://www.psychologytoday.com/blog/paintracking/201310/children-chronic-pain